The disease manifests as a sudden onset of severe headache, chills, pain upon moving the eyes, and low backache. Painful aching in the legs and joints (myalgias and arthralgias—severe pain that gives it the nickname break-bone fever or bonecrusher disease) occurs during the first hours of illness. The temperature rises as quickly as 40° C, with relatively low heart rate (bradycardia) and low blood pressure (hypotension). The dengue rash is characteristically bright red petechiae and usually appears first on the lower limbs and the chest (see Figure 2). The glands (lymph nodes) in the neck and groin are often swollen. In some patients, it spreads to cover most of the body. There may also be gastritis with associated abdominal pain, nausea, vomiting, or diarrhea. Some cases develop milder symptoms that can be misdiagnosed as influenza, chikungunya, or other viral infections when no rash is present. The classic dengue fever lasts about six to seven days, with a smaller fever peak at the trailing end of the disease (the so-called biphasic pattern). Clinically, the platelet count will drop until the patient’s temperature is normal.
Recognition of Dengue fever
- Sudden onset of high fever
- Severe headache (mostly in the forehead)
- Pain behind the eyes, which worsens with eye movement
- Body aches and joint pains
- Nausea or vomiting

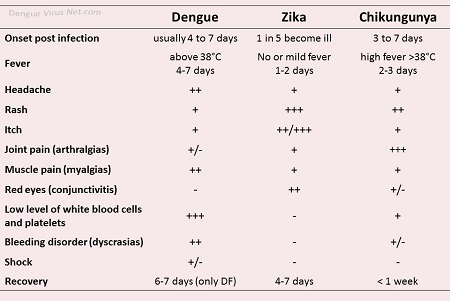
Dengue virus infections are sometimes confused with chikungunya viral infections because both diseases can present with high temperatures and myalgias (muscle pain) in people living in or returning from tropical areas (see Figure 2, and also diagnosis of Dengue and Chikungunya). Although these diseases share similar clinical features, prominent and prolonged joint pains are more consistent with chikungunya, whereas hemorrhage is more common in cases of dengue virus infection.